
GOING through a new-style CQC inspection can be a stressful and protracted experience, as those practices who have been inspected will know. It can take up to three months after the inspection to receive the draft report along with the proposed ratings. I am frequently contacted at this stage by practices who are of the view that the draft inspection report and ratings do not accurately reflect the standard of care they provide. What then follows is a process of challenge to the draft report which is finally published with an amended narrative and, very often, improved ratings.
However, the key question here is what can practices do to ensure that the draft report is "right" first time? There are a number of steps you can take to achieve this goal.
Understanding and complying with the CQC’s ‘fundamental standards’ is essential and goes hand-in-hand with having sound governance and assurance arrangements to monitor ongoing compliance and act on any issues arising. This should form part of the everyday business of any practice.
UNDERSTANDING THE BENCHMARK
In addition to understanding the legal requirements which make up the fundamental standards, practices need to keep up-to-date with how these standards are being interpreted and relevant inspection trends. Primary care organisations have secured the highest percentage of ‘good’ ratings among CQC-registered providers but there is no room for complacency. It is important for practices to keep up-to-date with published CQC reports and guidance to understand, for example, what makes the difference between ‘requires improvement’ and ‘good’. By reflecting on these trends and benchmarks, practices will be able to ensure that they avoid common pitfalls and stay on the right side of ‘good’ in regard to all five of the key questions considered in CQC inspections: is your practice safe, effective, caring, responsive and well-led?
For example, the table below contains a sample of the types of issues arising within the ‘safe’ domain.
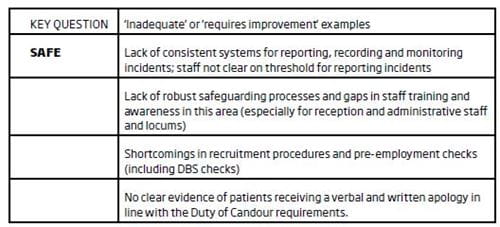
It is equally important to keep an eye on what ‘outstanding’ looks like. So in the ‘safe’ domain, evidence of "an open safety culture" and "comprehensive systems to keep patients safe from harm" will score highly with the CQC who will want to see significant events reviewed on a regular basis internally and externally (by bringing external stakeholders and multidisciplinary teams into the review meetings) before awarding the highest rating available.
This exercise can be carried out across all five domains. For example, issues arising in the ‘well-led’ domain might look like this:
KEY QUESTION: WELL-LED
Vision, culture and communication issues:
- Lack of succession plans in place for key staff, such as the practice manager or lead receptionist
- Lack of a clear vision and strategy
- Failure to involve key staff such as the practice nurse in plans to introduce new clinics
- No clear leadership structure and no whole-practice meetings
- Not all staff had received regular performance reviews.
Engagement and patient involvement:
- No adequate patient participation in the practice and no mechanism to obtain feedback from patients
- No systems to use complaints to improve the service delivered.
Governance:
- Absence of any recorded governance meetings
- No risk log or register to collate and mitigate relevant risk issues
- Policies undated/without a review date.
As for the ‘outstanding’ benchmark in the domain of ‘well-led’, this requires clear evidence of innovation in terms of the manner in which high-quality care is delivered, for example the development of bespoke clinics designed to meet the needs of a practice with a high student population (sports injury clinic, weekly drop-in clinic for patients with mild to moderate eating disorders and an allied CBT clinic). It is also important for the inspectors to find evidence of a clear vision and strategy to deliver high-quality care and for staff to understand this vision and their responsibilities in relation to it.
SUPPORT YOUR STAFF
It is clear from reading any CQC report that what staff say to inspectors carries a lot of weight and is frequently quoted in the inspection report. It is important to engage staff in the pre-inspection phase. They should all be clear about what a CQC inspection entails and have a high degree of familiarity with the five key questions and, ideally the key lines of enquiry (KLOEs) that underpin the questions. Staff should be supported in this regard so that they feel confident when speaking to inspectors and can present the most accurate information. Well-prepared practices will have a clear idea of the types of questions that the inspectors will ask their staff and will be confident that the responses given reflect the true position of the practice.
Most practices will have elements of outstanding and innovative care but these will not feature in the inspection report unless your staff, firstly, recognise these elements as outstanding and, secondly, speak up about them during their time with the inspectors. Starting this dialogue with your staff well in advance of any inspection will generate confidence and improve your chances of securing the right outcome in the inspection reports. You should also engage your patients in the inspection process and encourage them to get involved and have their say.
WORKING WITH THE CQC
The relationship you have with your lead inspector will be of fundamental importance in ensuring that the inspection process goes smoothly and also that the post-inspection phase is handled as efficiently as possible. You should ensure that you have an open line of communication with your lead inspector so that you can address any immediate issues arising during the inspection and can anticipate when the draft report may arrive.
A vital part of securing the right result for your practice is to ensure that the draft reports are factually accurate. The practice will have 10 working days to consider the draft report and make any factual accuracy submissions to the CQC. The CQC encourage providers to go further than just pointing out minor errors in draft reports; they expect providers to help them publish an accurate and fair report. Therefore, the new template supplied by the CQC invites practices to submit comments about the following:
- Typographical or numerical errors
- Challenges to the accuracy of the evidence set out in the draft report (providing evidence demonstrating the inaccuracy) and also describing any impact on the rating(s)
- Additional evidence which the practice considers should be taken into account in the report.
If the practice is not happy with the ratings proposed in the draft reports and believes these are based on inaccurate findings then this is the time to make these points. In practical terms, it will be too late to raise these issues after the 10-day factual accuracy period has closed. Ratings have been changed by the CQC in approximately 90 per cent of cases where we have supported providers through the factual accuracy process. If used correctly, this stage of the process can therefore deliver real results and those practices who are concerned about the accuracy of the draft reports cannot afford to miss this opportunity to put things right.
Where fair and valid concerns have been raised by the CQC then it is important to respond to these promptly and in a manner which will give the regulator the confidence that the practice can improve and does not need to be subjected to escalating regulatory or enforcement action. Again, the relationship with the CQC will be key at this stage.
It can be daunting to face a CQC inspection but the suggestions above should help you to take control of the process and lead from the front.
Ian Cooper is a partner at Capsticks solicitors, who have recently partnered with MDDUS to provide members with discounted legal advice on non-indemnity issues. Click here for more details
This page was correct at the time of publication. Any guidance is intended as general guidance for members only. If you are a member and need specific advice relating to your own circumstances, please contact one of our advisers.
Read more from this issue of Practice Manager
Save this article
Save this article to a list of favourite articles which members can access in their account.
Save to library