 THE provision of implant dentistry in the UK
has been rising for some years and so has the
number of patient complaints associated with
this treatment modality. This is likely to be
related both to the costs and complexity.
THE provision of implant dentistry in the UK
has been rising for some years and so has the
number of patient complaints associated with
this treatment modality. This is likely to be
related both to the costs and complexity.
Implant dentistry is not yet recognised as a specialty by the General Dental Council, but it is a mode of treatment for replacing missing teeth which does require specific training. The main areas where practitioners face challenges to their care are largely related to competency and training, adequate assessment, treatment planning and consent.
Competency
Dentists contemplating implant training can find more details in the Faculty of General Dental Practice’s (FGDP) Training Standards in Implant Dentistry. Be sure your course is well structured with an adequate balance between theoretical teaching and mentored clinical experience. The value of mentoring cannot be under-estimated and is the key to ensuring a safe and competent practitioner.
Practitioners whose training pre-dates existing formal courses should be able to demonstrate their training and experience, ideally with a portfolio. Such a portfolio, which should also be maintained by those with formal training, will form the foundation of evidence that a practitioner was competent to undertake implant treatment in the first place. Additionally, a practitioner needs to provide care within their skillset and be aware of when it is appropriate to refer.
Full assessment
Assessing the medical history is of paramount importance. It is especially important to identify smokers, patients with diabetes, patients on medications that affect bone metabolism and bleeding tendency.
The failure to carry out a full mouth assessment and instead focus solely on implant treatment leaves a dentist vulnerable to allegations of poor treatment. This includes addressing caries, periodontal disease and considering the prognosis of other teeth.
Not managing primary disease before embarking upon implant treatment creates the potential for problems further down the line. Patients can become unhappy when they have paid large amounts for implant treatment but then find there were other treatment needs that were not addressed. For example, if an anterior implant bridge was carried out but caries in other teeth were not managed, leading to their early loss, a patient could rightly consider that a different treatment plan would have been more appropriate from the outset.
Periodontal risks
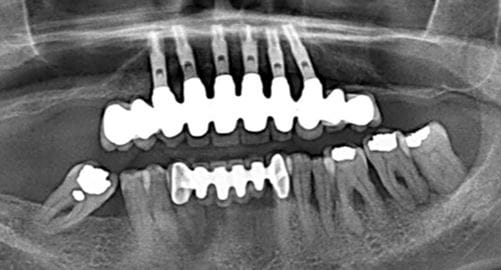
Implant provision in periodontally compromised patients requires particular mention. It is accepted that periodontitis is a risk factor for peri-implantitis and therefore for the failure of implants. It is essential that a proper periodontal assessment is carried out and periodontal care provided that is appropriate to that assessment, before embarking on implant treatment.
The advice given in The Good Practitioner’s Guide from the British Society of Periodontology is still the accepted standard for periodontal care. If the services of a hygienist are to be used, the dentist leading the care must maintain responsibilities for diagnosing and treatment planning the periodontal condition. Cases involving a failure to adequately manage a patient’s periodontal condition before implant treatment can lead to large settlement sums. Post-treatment monitoring of peri-implant tissues is also essential for early detection and management of peri-implantitis. There needs to be a clear understanding whose role this will be in the case of referral patients, since monitoring of these tissues can often become the responsibility of a GDP.
Coordinating care
When more than one practitioner is involved in patient care, it is important to understand who has responsibilities for what aspects of care. Examples are when a patient is referred to another practice for implant treatment or when a patient self-refers solely for implant treatment - or where different practitioners carry out the surgical and prosthetic implant treatments. Without a clear understanding of where responsibilities lie (and in the case of a complaint relating to treatment planning) all practitioners involved in the patient care could become liable to some extent. In the case of different dentists carrying out the surgical and prosthodontic aspects of implant care it is essential that both practitioners agree what is possible to achieve in a particular case, and communicate this to the patient.
Consent
Consent is a vital component of healthcare delivery. In the first instance, valid consent requires that the patient is competent and un-coerced. The patient must also be sufficiently informed about the procedure and alternatives, together with their material risks, benefits and costs.
Alternatives might include bridges or dentures. There might also be a number of implant-based solutions. These treatments must, in the opinion of the practitioner, be clinically justifiable before being placed on the consenting menu.
Risks are those which the reasonable patient in these particular circumstances would regard as significant. Exploration of this issue necessitates bespoke, interactive dentist-patient discussions. Where a highly technical subject is being planned, particular consideration should be given to the comprehensibility of this information. Patients should be given time to reflect on this advice and should be allowed to return with any ongoing concerns.
Written consent for implant treatment is not mandatory, unless sedation or general anaesthesia is provided. However I cannot over-emphasise the importance of providing written information, as long as it has been properly drawn up, as a way of ensuring that information has been provided. In order to ensure consent is valid there needs to be patient understanding and therefore I must also caution against solely relying upon giving written information for the purpose of obtaining consent. It is essential that the practitioner spends time in verbally checking that the patient understands the information provided, even if it has been given in writing, and allow sufficient time for the patient to consider the information. Furthermore, provision of written information should be as patient-specific as possible.
Part of valid consent is to ensure that the patient is aware of the expected end result. This is particularly important where there is an aesthetic element. Time spent with models, photographs and diagnostic wax-ups at the outset will help to ensure there are no unexpected surprises at the end of treatment.
The provision of a written treatment plan and an estimate of costs is, however, mandatory. This becomes crucial where the treatment is complex with multiple phases, or the plan (and consequently the costs) change during treatment.
Good clinical records are essential to evidence the care and discussions provided. Computer-driven templates are useful in making this process more efficient, but the dentist must ensure that all the information contained in pre-designed templates apply to the individual patient.
Dr Abhi Pal is a GDP who carries out implant dentistry and is currently vice-dean of FGDP(UK). He is frequently called upon by defence organisations, the GDC and clinical negligence lawyers to provide independent expert advice in complaints related to implant dentistry
ABOVE: Implant treatment carried out in upper arch without addressing periodontal disease in lower arch (PHOTO: ABHI PAL)
This page was correct at the time of publication. Any guidance is intended as general guidance for members only. If you are a member and need specific advice relating to your own circumstances, please contact one of our advisers.
Read more from this issue of Insight Primary
Save this article
Save this article to a list of favourite articles which members can access in their account.
Save to library