BACKGROUND
Mr T attends his GP surgery complaining of a mole on his chin that has been present for at least 10 years. He has grown increasingly unhappy with the appearance and finds it gets easily nicked when he shaves.
The GP, Dr J, examines the lesion, notes that it is reddish-brown and 7mm in diameter. She records “nothing suspicious”.
Mr T wants the mole removed but Dr J explains this would not be available on the NHS, as it is for cosmetic reasons, and offers to make a private referral.
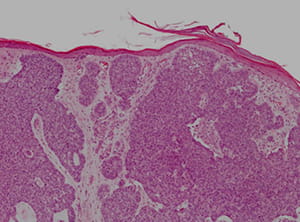
An appointment is arranged two months later with a consultant dermatologist at a private clinic. The lesion is removed and a subsequent biopsy reveals a diagnosis of basal cell carcinoma. No further treatment is provided and the surgical wound heals well.
Six months later Dr J receives a letter from the General Medical Council (GMC) in regard to concerns that have been raised over her fitness to practise in connection with the clinical care of Mr T.
It is alleged that Dr J failed to consider a diagnosis of basal cell carcinoma and refer the patient for further investigations. The concerns do not meet the threshold to open a formal investigation and the GMC instead consider the matter under their provisional enquiry rules.
The GMC investigation officer also sends Dr J an Employer Work Details form to complete, providing details of her responsible officer and where the alleged incident took place, as well as other information about the scope of her work. An expert opinion based on the patient records will be commissioned to help determine if the matter needs to be investigated further.
The letter further advises that Dr J can provide comments on the allegations and recommends she take advice on this from her medical defence organisation.
Dr J writes back immediately to the GMC detailing what she recalls of the consultation and justifying her belief that on balance the lesion was non-cancerous. She expresses her sincere regret for the perceived delay in diagnosis.
ANALYSIS/OUTCOME
Dr J contacts MDDUS a few days later and a medico-legal adviser and an inhouse lawyer take on management of the case.
Dr J is advised that in future she should seek MDDUS advice before replying to GMC correspondence, as MDDUS are able to offer expert help in how to draft a response. It is proposed that (given Dr J has already submitted her comments) no further comment is offered to the GMC at this stage, and a plan is agreed to wait and see what comments the GMC expert makes following their review of Dr J's care.
A few months later the GMC writes to Dr J to inform her that the provisional enquiry has been completed and no investigation will be undertaken. An appendix to the letter provides further details on the reasoning behind the decision.
The independent expert assessing the evidence found that the standard of care provided by Dr J fell below, but not seriously below, that expected of a reasonably competent GP. A potential diagnosis of skin cancer should have been considered but based on what was written in the notes there was no indication for a biopsy. Mr T expressed a desire to have the lesion removed for cosmetic/convenience reasons and the private referral was appropriate in the circumstances.
The expert however did comment on the paucity of the clinical records and no mention of safety netting.
The GMC further states that the matter is something that should be reflected upon as part of Dr J’s appraisal and that a copy of the letter has been passed to her responsible officer.
KEY POINTS
- Ensure patient notes reflect the full history/clinical examination and justification behind clinical care decisions.
- Provide and record safety netting advice.
- Contact MDDUS for advice before responding to correspondence you receive from the GMC.
This page was correct at the time of publication. Any guidance is intended as general guidance for members only. If you are a member and need specific advice relating to your own circumstances, please contact one of our advisers.
Read more from this issue of Insight Primary

Save this article
Save this article to a list of favourite articles which members can access in their account.
Save to library