THE term evidence-based medicine was first introduced into medical literature in 1991, with a focus on assessing the validity and importance of evidence before applying it to day-to-day clinical problems. Since then it has been adopted by other health disciplines including dentistry.
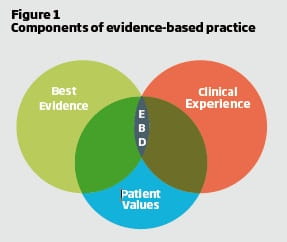
The American Dental Association (ADA) defines evidence-based dentistry (EBD) as “an approach to oral healthcare that requires the judicious integration of systematic assessments of clinically relevant scientific evidence, relating to the patient’s oral and medical condition and history, with the dentist’s clinical expertise and the patient’s treatment needs and preferences.”
Putting this simply it means bringing together the best available evidence on a topic with the dentist’s expertise and the patient’s needs and wishes (Figure 1) in order to deliver the right treatment in the right way at the right time and at the right place. While the best clinicians have always sought to practise in this manner, the explosion of information available and the pace of development mean that keeping up-to-date is increasingly challenging. Adopting an evidence-based approach helps manage this information overload.
Evidence-based practice is a systematic approach for dealing with this vast amount of information by providing methods for aggregating, distilling and delivering the best clinical evidence. The five stages have been referred to as the five As:
- ASK - ask answerable questions
- ACQUIRE - find the best evidence
- APPRAISE - critically appraise the evidence
- APPLY - apply the evidence
- ASSESS - assess the outcome
Ask
Consider the following scenario:
A family attends for a routine check-up on your first day in a new practice. When you examine the mouths of the two young children you diagnose caries in some teeth. On questioning to establish possible risk factors, the mother indicates that they brush their teeth twice a day with herbal toothpaste as they live in a fluoridated area. You ask the mother if the toothpaste contains fluoride and she confirms that it does not.
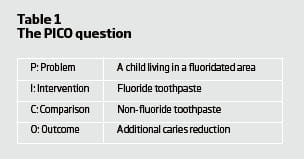
You can probably think of a large number of clinical questions related to this scenario but an important one for me is whether changing to fluoridated toothpaste would be beneficial. To help develop clear questions to aid searching for evidence a format called PICO has been developed1. This stands for problem, intervention, comparison and outcome. For the scenario above we could derive the following question: For a child living in a fluoridated area would fluoride toothpaste, compared with a non-fluoride paste, provide additional caries reduction? Armed with a clear question we can then look for the best evidence to answer it.
Acquire
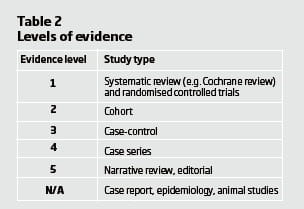
Before looking for evidence it is important to realise that not all evidence is of equal value. Essentially you are looking for the research that is best designed to suit the question you are trying to answer2. For a question seeking to find out if one treatment is better than another, a systematic review of randomised controlled studies is the highest level of evidence, and this decreases based on the potential for bias within the study design as shown in Table 2. (More information on levels of evidence is available on the Centre for Evidence-based Medicine website)
In an ideal world we would conduct our own systematic review of the evidence but this is unrealistic. The simplest approach is to look for some form of pre-appraised evidence. This can come in a number of different formats3 as shown in Table 3.
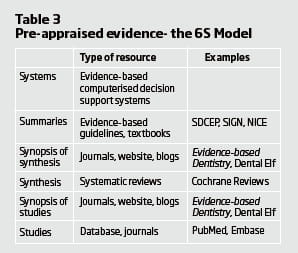
While a formal search of evidence using the resources noted in the table would be best practice (and a useful skill to develop), from a practical perspective good evidence-based guidelines such as those prepared by the Scottish Dental Clinical Effectiveness programme (SDCEP) and Scottish Intercollegiate Guidelines Network (SIGN) and journals and blog sites that produce summaries of good quality articles such as the Evidence-based Dentistry journal (of which I am editor) and the Dental Elf blog are good starting points when looking for evidence. Another time-saving approach is to use the TRIP database. This is a meta-search engine that automatically searches a range of the resources noted in Table 3 and allows you to select a particular type of resource.
Searching is a key skill to support the evidence-based approach. Without a good search for information to answer your question there is a temptation to use the first available piece of evidence to support an approach to treatment and claim that this is “evidence-based” when in fact it is neither good evidence nor the only treatment approach available.
Appraise
Once you have found your evidence you need to appraise it. There are a range of appraisal tools and checklists to help with this element. The most useful of these are produced by the Critical Appraisal Skills Programme which has checklists for a range of different study designs. Regardless of the study design, there are essentially three core questions to address:
- Is the study valid?
- What are the results?
- Are the results relevant to my patients?
When appraising most studies the validity or correct methodology is key and most people can assess this for themselves most times.
Apply and assess
So once you have identified the evidence and have assessed it as sound and relevant to your patient you need to discuss it with your patient. This is particularly important if there are options for care, as the evidence-based approach also includes taking the patient’s needs and values into consideration. Finally, once the treatment has been delivered you should assess whether your experience with the treatment is the same as the evidence on which you based your decision-making in order to complete the loop.
Talking of completing the loop, in relation to the question we asked at the outset, probably the best evidence comes from a Cochrane review by Marinho et al4, which found that fluoride toothpaste provides about a 24 per cent reduction in dental decay, and that this effect was increased with higher disease levels, high toothpaste fluoride concentration, higher frequency of use and supervised tooth brushing, but not influenced by exposure to water fluoridation.
References
- Richardson W, Wilson M, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions [editorial]. ACP J Club. 1995; 123: A12-13.
- Sackett DL, Wennberg JE. Choosing the best research design for each question. BMJ. 1997; 315: 1636.
- DiCenso A, Bayley L, Haynes RB. ACP Journal Club. Editorial: Accessing preappraised evidence: fine-tuning the 5S model into a 6S model. Ann Intern Med. 2009; 151: JC3-2, JC3-3.
- Marinho VC, Higgins JP, Sheiham A, Logan S. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003; Issue 1. Art. No.: CD002278. DOI: 10.1002/14651858. CD002278.
Derek Richards is an honorary senior lecturer at the University of Dundee Dental School, consultant in dental public health, and director of the Centre for Evidence-based Dentistry
This page was correct at the time of publication. Any guidance is intended as general guidance for members only. If you are a member and need specific advice relating to your own circumstances, please contact one of our advisers.
Read more from this issue of Insight Primary

Save this article
Save this article to a list of favourite articles which members can access in their account.
Save to library

