AS A DOCTOR you are used to caring for patients on an individual basis – but what about a specialty that lets you make an even bigger impact by protecting the health of entire populations?
Public health offers the chance to positively influence the health of large numbers of patients by doing everything from promoting healthy behaviours to tackling the health effects of climate change across the country.
An estimated 40,000 people work in core public health roles across the UK, but this number rockets to as high as 20 million when taking into account the wider workforce such as dental teams, pharmacists, midwives, district nurses and beyond.
It is a formidable number, yet there are still considerable health challenges to be tackled. There are many opportunities for those seeking a career as a public health specialist or consultant.
Entry and training
Doctors interested in a career in public health normally apply for specialty training after completion of their two-year foundation training. This is a competitive process with an average of 500-600 eligible applicants annually for 70-80 places. NHS Health Careers offers tips for getting into training which include joining the Faculty of Public Health (FPH), seeking work experience at a local public health organisation and attending conferences on public health. Trainee doctors are also encouraged to undertake a rotation in public health or to use study leave to undertake a taster programme.
Specialty training normally lasts five years, culminating in the award of a certificate of completion of training (CCT) in public health medicine. The pathway is divided into two phases. In phase 1, trainees gain public health knowledge and core skills and obtain the part A and part B exams. In phase 2, trainees have the option to select special interests and take on increasing levels of responsibility. It is also at this point when trainees can apply for time to undertake a PhD, two years of which may count towards a CCT. Movement between phases is dependent both on exam success and achievement of learning outcomes.
The FPH sets out the three key domains of public health practice which relate to:
- health improvement – e.g. inequalities, education, housing and behaviours
- improving services – e.g. audit and evaluation, service planning and clinical governance
- health protection – e.g. infectious diseases, emergency response and environmental health hazards. In addition, they detail nine key areas which are covered in training. These include: surveillance and assessment of the population’s health and wellbeing
- assessing the evidence of effectiveness of health and healthcare interventions, programmes and services
- policy and strategy development and implementation
- strategic leadership and collaborative working for health
- health improvement
- health protection
- health and social service quality
- public health intelligence
- academic public health.
According to Health Education England’s specialty training site, applicants should be able to show an understanding of public health concepts and inequalities. They should also have a political awareness and understanding of the impact of national policy on health, and have a basic understanding of research methodology.
The job
The FPH defines the field as: “The science and art of promoting and protecting health and wellbeing, preventing ill-health and prolonging life through the organised efforts of society.”
Public health specialists and consultants are described by NHS Health Careers as “strategists or senior managers or senior scientists”, working across all three domains of public health. They will usually be employed primarily within local authorities or national agencies such as Public Health England. There are also opportunities within the NHS, the prison service, Defence Medical Services, think tanks, voluntary organisations and even bodies such as the National Institute for Health and Care Excellence (NICE). The private sector also hires specialists within companies, organisations, and consultancy firms.
The job as a specialist/consultant is varied and includes responsibilities such as working with senior colleagues on the planning and delivery of policies and programmes to influence the health of groups of people at local, regional and national levels. They will also provide professional, evidence-based advice on the commissioning of services to improve health and wellbeing and reduce health inequalities across primary, secondary and social care. One potential role is that of consultant epidemiologist, providing strategic leadership in the surveillance of infectious diseases and environmental hazards.
Public health academics usually work in universities or further education, in the UK or abroad, across all three domains. NHS Health Careers describes how they typically set up research investigations to address specific public health issues. They may also teach about public health theories and practice. Their day-to-day work is likely to consist of: teaching; assessing and examining students’ work; researching public health issues; and sharing the results of their work. Roles include research assistant, academic clinical fellow, research fellow or clinical lecturer.
Sources:
 Q&A
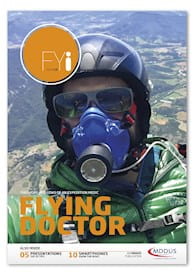
Dr Rachael Hornigold,
public health specialty
registrar, Extreme
Events, Public Health
England
Q&A
Dr Rachael Hornigold,
public health specialty
registrar, Extreme
Events, Public Health
England
What first attracted you to public health?
I initially trained in ENT surgery, and was a long way through my higher surgical training when I became interested in public health. I had had very limited exposure to public health at medical school or in my initial training placements but became aware of the training scheme when I worked with public health consultants on a service redesign. I absolutely loved the experience and after some shadowing placements decided to apply for public health training.
What do you enjoy most about the job?
I really enjoy the multi-disciplinary nature and the chance to get involved in vastly different projects well outside the usual medical sphere. In the last year I’ve directed a video for healthy eating with nursery children, attended crossdepartmental meetings on climate change in Whitehall, worked with the Met Office on cold weather alerts and dealt with infectious disease outbreaks. I also enjoy the ability to manage my own workload in the way that works best for me.
What do you find most challenging?
The breadth of public health is massive – so it is a challenge to stay up-to-date with developments in the field. The membership exams are challenging, but you are offered lots of support, including the opportunity to undertake a master’s degree in public health.
Has anything surprised you about the specialty?
Public health specialist training is the only training scheme that accepts applicants at ST level who are non-medics. So you may find yourself training with dentists, vets, nurses and people with a complete lack of medical training, such as those with a background in politics, policy and health promotion. This leads to a very diverse and interesting group of colleagues, with their own individual strengths and knowledge base.
What do you consider the most important attributes of a good public health specialist?
The ability to quickly become a subject area specialist at short notice, the ability to be flexible in your role and to be a team player, appreciating all of your colleagues’ skills and experience.
Is there any advice you could give to a final year or FY trainee considering public health?
There is limited clinical work in public health so you need to be very sure this suits you. It may be useful to undertake additional clinical placements before applying. Contact your local authority team and your local health protection team to speak to registrars and consultants about what they do day-to-day and potentially organise some shadowing. The FPH website is a great source of information.
This page was correct at the time of publication. Any guidance is intended as general guidance for members only. If you are a member and need specific advice relating to your own circumstances, please contact one of our advisers.
Read more from this issue of FYi
Save this article
Save this article to a list of favourite articles which members can access in their account.
Save to library
