
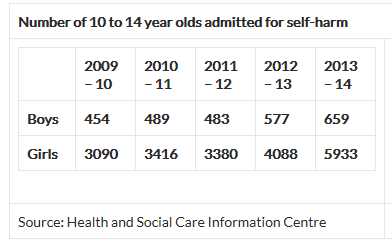
A recent report published by the Health and Social Care Information Centre highlighted that the number of children (10 –14 year olds) being admitted to hospital in England for self-harm is at a five-year high, with admissions of girls increasing by almost 93 per cent and a rise of 45 per cent in boys.
Mental health campaigners believe the figures could be the tip of the iceberg. Boys are often reluctant to admit to self-harming because it is perceived as a largely female behavioural problem and as a result they fear "huge numbers" of children - especially boys - are still "suffering in silence".
Experts say that increases in admissions are partly due to a rise in young people self-harming, but also reflected better recording of data by hospitals. They argue that a ‘cultural shift’ is needed in society to ensure teachers and parents are not afraid to address the topic of self-harm, particularly among boys.
The report explores further social reasons for the gender discrepancy in young people seeking help, suggesting that because of the way society has constructed the image of self-harming, it makes it easier for girls to speak out about the problem.
Self-harming behaviour of course, represents only one reason why a young person may consider approaching their GP for help. And by ‘young person’, I am referring to the very age group studied in the report, those that are in the often difficult transition between childhood and adulthood.
The legal and ethical dilemma here for a health professional, of course, is one of competence and when a young person can demonstrate sufficient emotional maturity to make decisions about their own health and well-being without the involvement of their parents or other guardians. Fortunately, health regulatory bodies – such as the GMC in their 0-18 publication along with the Caldicott Information Governance Review - and other professional organisations provide plenty of guidance in this area, without of course providing answers and solutions to situations which are set in tablets of stone.
Even before a young person gets to the stage where they are in position to have an intelligent one-to-one consultation with their doctor, dentist or other health professional, I wanted to consider and explore another important consideration. Just how young person-friendly is your own practice or service?
Assuming that your service does not operate a deliberate policy of dissuading young people from seeking medical help and assistance, I wanted to look at some of the more common areas where practices are promoting positive incentives for ease of access, and highlight some of the negative aspects that we have come across in this area.
For example, does your service actively promote itself to young people? By this I mean through the use of specific literature including, where applicable, web-based info with links. Does this reflect the style of language used to communicate between this age group? Or, conversely, does the information and welcome you provide to young people suggest that it is actually discouraged?
Young people should be reassured that the principle of confidentiality extends beyond health professionals to other staff (such as receptionists), who may live locally and have social relationships with the young person’s extended family. The erroneous presumption that confidentiality does not extend to other staff in itself could be a compelling reason for a young person not to consult with their GP.
We have come across instances where written information states that under 16s need to be accompanied by an appropriate adult! This is a capacity and competence issue first and foremost, and the young person’s ability to make decisions for him/herself should be considered from the outset, before determining how involved parents should be.
Have you considered how the reception team handle calls requesting appointments from a patient who is under 16, and are they aware of the potential sensitivities around screening reasons for wishing to see the doctor?
The practice can show they understand the particular problems young people can face by publicising in their waiting room examples of why they may wish to see a doctor:
- If you feel down all the time
- Are you being bullied at school?
- If you have condition you find embarrassing
- If you have unprotected sex, or you wish to discuss contraception
- Are you concerned about your weight?
Another example of proactive policy and practice that we have encountered is where the service addresses this issue directly with parents, when the young person reaches around 12 years of age. This can take the form of a standard letter informing parents that, as their child matures, they will be increasingly able to make decisions about their own care and treatment. This will mean that individual approaches by the young person will be assessed according to the circumstances, meaning that parents may not automatically be informed about the contact.
Understandably, some services are reluctant to address this issue head-on for fear of opening a can of worms, as most parents will be quite forceful in exercising what they see as their legitimate ‘parental rights’. However, having the conversation at a stage where there is no ongoing crisis with the accompanying emotional baggage, can be more beneficial in the long run. At the very least it will have hopefully planted a seed in the parents’ mind and allow them to consider the issue and its implications.
We would be interested to hear of any practical ideas that your service employs to address this particular issue.
This page was correct at the time of publication. Any guidance is intended as general guidance for members only. If you are a member and need specific advice relating to your own circumstances, please contact one of our advisers.
Save this article
Save this article to a list of favourite articles which members can access in their account.
Save to library